The evolving battle of vaccine versus coronavirus
EXPLAINER
COVID-19 mutations are fuelling a medical arms race, writes Liam Mannix.
Somewhere in the world, there is a person who is very, very sick. Perhaps they have leukaemia, a cancer of the blood, treated with chemotherapy. Perhaps they have an autoimmune disease, so doctors are pumping drugs into their system to stop their immune system attacking their body. Or maybe they have battled a rattling cough and lethargy for months.
Different cases with a common thread: their immune systems are exhausted, their defences down.
Such people are one possible origin story for the coronavirus variants across the globe.
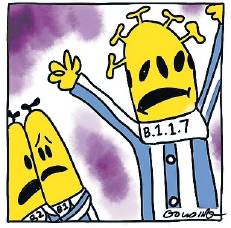
First, B.1.1.7 was linked to a dramatic increase in cases in Britain; an escaped case sent Brisbane into a snap lockdown. South Africa is facing a surge from a variant known as N501Y.V2. A third, more mysterious, variant, is linked to a spike of infections in a Brazilian city thought to have achieved herd immunity.
In an effort to keep the variants out, the federal government halved some international arrival caps on January 8. The rise of variants is an expected part of any viral pandemic. But these viruses caught scientists by surprise and now threaten to accelerate the pandemic even as countries race to vaccinate their populations.
Is it a mutant, or a new strain?
A mutation is a random change in an organism’s genetic code, when one of the letters of the code is switched out for another as the code is copied, when a virus replicates. Often, these changes have no effect on the organism hosting the virus.
A variant is a virus with a collection of mutations – such as B.1.1.7 – that turns up often enough for scientists to take an interest. That’s different from a strain, which denotes essentially a whole new virus type, or a virus that has changed so much it causes different symptoms. B.1.1.7 is a variant of SARS-CoV-2 and SARS-CoV-2 is a strain of coronavirus.
Where did variants come from?
As late as December 13, British health officials thought they had some measure of control over their epidemic. On that day, the country recorded 21,988 new cases and 419 deaths. But soon after, daily cases peaked at 81,520. Much of the country was pushed into tier-four lockdown. Driving much of that surge, Prime Minister Boris Johnson said, was a new and fastspreading variant of COVID-19 known as B.1.1.7. A mutant.
B.1.1.7 emerged in the academic literature as a footnote, a variant slotted into a widening family tree as scientists sequenced the viral genomes from sick Britons. The first genomic report to mention it found just two samples. Genomic databases would later show the first sample was taken in Kent on September 20.
But B.1.1.7 wasn’t just another member of a growing family. When you draw a COVID-19 family tree, it has so many mutations it sticks right out like a rogue branch.
In late November, three testing labs in England started to report strange results from some COVID-19 tests. These tests targeted three genes in the virus, including one coded for the virus’s spike protein. The tests showed positive for two of the genes, but the spike was blank. A malfunction in the test, perhaps? But the malfunctioning test numbers kept growing.
Other scientists were investigating B.1.1.7’s rogue tree branch. The virus had amassed 17 mutations, far more than scientists would expect in such a slowmutating virus. Eight of those were to the spike protein, subtly changing its shape. One mutation, scientists realised, would cause standard COVID-19 tests to miss the spike.
That’s what the testing labs were seeing. The tests weren’t malfunctioning. B.1.1.7 was everywhere. By the week of December 9, B.1.1.7 made up 62 per cent of cases in London.
Britain was in the middle of a viral surge so scientists expect to see more cases of all variants. But B.1.1.7 was growing fast, outcompeting its cousins.
University of Sydney virologist Professor Edward Holmes told the ABC: ‘‘The compelling thing is it is not just spreading rapidly in itself, but it is replacing all the other strains in the population. And that suggests it has some advantages: it’s fitter, it’s doing better, it’s transmitting more readily.’’
It has now spread around the world. Australia has recorded 51 cases so far.
What are the differences?
Scientists are most concerned by three variants of COVID-19: B.1.1.7, first spotted in Britain, 501Y.V2, first spotted in South Africa (also referred to as B.1.351) and P.1, first spotted in Brazil.
Under an electron microscope, all these viruses look identical: little spheres covered in spikes.
To infect a human cell, one of those spikes needs to fit into a slot on a human cell, a receptor called ACE2.
The virus that emerged out of Wuhan wasn’t very good at doing that. Often, the spike would bounce off its target, or slip out of its grip.
The new variants are much improved. All three possess a mutation called N501Y, which slightly changes the shape of the tip of the spike, allowing it to bind tighter to human cells. There is now significant evidence that B.1.1.7, at least, is substantially more transmissible. The South African and Brazilian variants add a pair of mutations, K417T and E484K, which hide part of the spikes targeted by human antibodies.
These mutations are of concern as there is evidence they reduce the effectiveness of antibodies, a tool of the immune system and of vaccines.
Were we expecting mutations?
The new mutants were, to an extent, unexpected. Viruses naturally mutate, as changes in their genetic code accumulate. Since it left Wuhan, COVID-19’s family tree has branched and branched until the original virus is almost undetectable. Everything is variants.
The chance of a virus evolving to be fitter – more transmissible, better at avoiding immunity – was 100 per cent, Burnet Institute director Brendan Crabb wrote on Twitter. ‘‘And it was 100 per cent predictable the more virus there is, the faster this would occur.’’
But COVID-19 is slow to change, about two to four times slower than the flu, says Dr Sebastian Duchene, who studies viral evolution at the Peter Doherty Institute for Infection and Immunity. That’s because, unlike the flu, it incorporates a genetic proofreader that picks up typos in its code.
It has shown perhaps one or two mutations a month. At that rate, pandemic-altering mutations seem unlikely. But B.1.1.7 and the other variants have more changes than that. The variant spotted in South Africa, 501Y.V2, has nine changes to its spike protein alone. P.1, the Brazil variant, has 20 changes, including three in the spike.
These variants appear to have outpaced evolution. How?
Says Kirby Institute virologist professor Stuart Turville: ‘‘We do not know but the rapid appearance of these changes is faster than expected.’’
One leading theory: immunocompromised patients.
As they have no immune system to mount a defence, COVID-19 could live inside them for months, replicating again and again, rapidly accelerating evolution.
They may even have been treated with convalescent plasma, which contains antibodies from recovered patients; it would wipe out all variants of the virus except any lucky enough to have randomly developed resistance. Empowered with new mutations and unhindered by competition, that virus could spread.
Several of these patients, their bodies filled with mutation-carrying viruses, have been found – although no patient zero yet.
Why would these ultra-rare events happen now? The simple maths of probability: the more infections you have (we just passed 100 million cases worldwide) the more chance of an extremely rare event happening.
What’s the likely effect?
One theory promoted by opponents of lockdown – and officials appointed by former US president Donald Trump – is that natural herd immunity will bring the virus under control. Once enough people have been infected and have developed antibodies, the virus will have nowhere to go and it will die out.
Ground zero for that idea: Manaus, Brazil. In September, scientists suggested the city had reached herd immunity, as 66 per cent of the population had antibodies to COVID-19 (the cost: thousands of deaths).
With so many people immune, Manaus should largely have had COVID-19 under control, the thinking went. Instead, in mid-December the virus again started racing through the city. Its hospitals became more packed than during the first wave; some are running out of oxygen and ventilators.
What’s gone wrong? One theory: a mutant. In late December, scientists identified a new variant, P.1, containing an array of mutations that, in the South African variant, seem to convey significant antibody resistance.
A non peer-reviewed South African study tested the blood of 44 patients who had recovered from COVID-19, and therefore should theoretically have been immune, against the South African variant. Some 21 had no detectable neutralising antibody activity.
Scientists don’t yet know if that means they are vulnerable to infection. Burnet Institute epidemiologist professor Michael Toole says: ‘‘Neutralising antibodies are only one part of our immune response. Scientists will [also] be looking at T cell responses.’’
But it’s not a promising sign.
Are the mutations more deadly?
It is unclear if the variants are more likely to cause injury or death. On January 23, Britain’s chief medical and scientific officers said they had emerging evidence B.1.1.7 was more deadly. Government advisers can say only there is ‘‘a realistic possibility’’ the virus is more deadly.
Will this affect the vaccine?
When our immune system encounters a pathogen, it makes many different shapes of antibody. Some don’t work. Some work partially. And some bind perfectly. A small change in a virus’s shape might allow it to evade one antibody, but others should still block it.
B.1.1.7 has nine changes to amino acids on its spike protein out of more than 1270. There is still plenty there to grab on to. It takes a string of mutations to fully evade antibodies; so far, we have evidence only the South African variant might be able to do this.
That does not mean any variant can evade vaccines. Pfizer, Moderna and AstraZeneca jabs generate such a strong immune response that scientists expect, even if the new variants can partially resist them, they will still be covered.
The early laboratory evidence shows the new variants modestly cut, but do not fully cancel, the efficacy of the vaccine.
But two human trials just released may undercut that. As part of phase three trials, first Novavax and then Johnson & Johnson reported their vaccines were less effective, as low as 49 per cent, against the South African variant.
Several companies are working on boosters to cover the variants. But it’s another development that has scientists concerned.